CONDITIONS
SYMPTOM CHECKER
Male
Female
Child
Arm, Hand & Shoulder Concerns
Legs & Feet Concerns
Dental & Mouth Concerns
Ear & Nose
Eye Conditions
Head Conditions
Arm, Hand & Shoulder Concerns
Legs & Feet Concerns
Front
Back
Arm, Hand & Shoulder Concerns
Dental & Mouth Concerns
Ear & Nose
Eye Conditions
Head Conditions
Arm, Hand & Shoulder Concerns
Dental & Mouth Concerns
Ear & Nose
Eye Conditions
Head Conditions
Front
Back
Arm, Hand & Shoulder Concerns
Neck Links
Head & Neck Concerns
Arm, Hand & Shoulder Concerns
Neck Links
Head & Neck Concerns
Front
Back
Online Clinic
Wise Healthcare
Asthma
Asthma is a chronic disease that causes the airways to narrow. Airflow is limited due to inflammation in the airways.
Wheezing
Symptoms
Causes & Risk Factors
• Genetic Factors. You are more likely to have asthma if other members of your family have or had it.
• Environmental Factors. Being exposed to certain things can set off an immune system response for asthma to develop. Examples are house-dust mites and viral respiratory infections.
Diagnosis
A doctor diagnoses asthma from:
• Your medical history
• Your family’s medical history
• Your symptoms
• A physical exam
• Lung function tests in persons age 5 years and older
• Other tests to check for conditions that have symptoms of asthma, but are not asthma
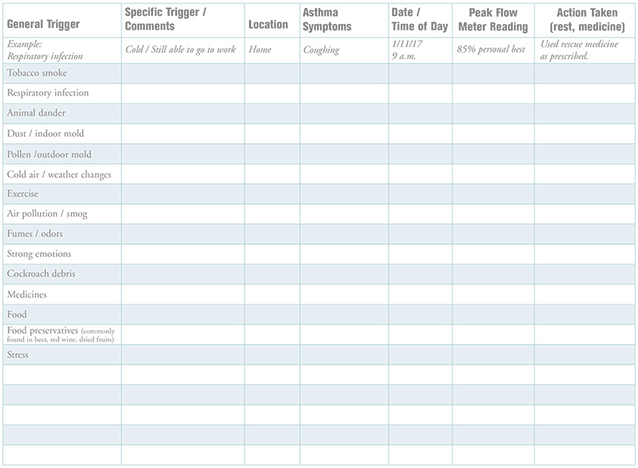
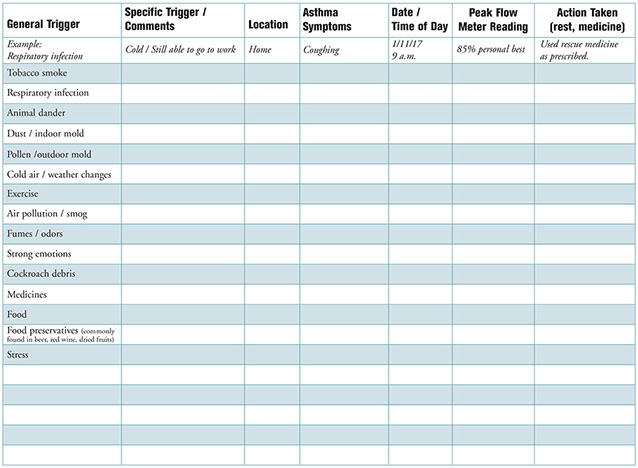
Asthma Attack Triggers
People with asthma have very sensitive airways. Exposure to triggers causes a response in the airways called an asthma attack or an asthma episode.
Resources
The Asthma and Allergy Foundation of America
800.7.ASTHMA (727.8462)
National Heart, Lung, and Blood Institute
301.592.8573
With an asthma attack:
• Air becomes trapped in the lungs.
• The lining of the airways becomes inflamed.
• The muscles around the air tubes tighten.
• Thick mucus clogs the airways.
(The last three things cause the airways to narrow.)

Problems That Make It Harder to Manage Asthma
• Reflux of stomach acids which cause heartburn, belching, or spitting up
• Being overweight or obese
• Allergic rhinitis or sinusitis
• Sleep apnea that obstructs breathing
• Stress and depression
Treating these problems may help improve asthma control.
Common Asthma Attack Triggers
• Respiratory infections (colds, flu, bronchitis, etc.)
• Tobacco smoke
• Dust mites
• Animal dander (small pieces of skin, hair, or feathers from warm-blooded animals, such as dogs, cats, birds, etc.)
• Cockroach droppings
• Molds (indoor and outdoor)
• Strong odors and sprays from paints, new carpet, perfumes, etc.
• Air pollution
• Cold air and changes in temperature and humidity. Weather changes can also affect how much pollen and mold are in the air.
• Having strong feelings (laughing, crying, etc.)
• Sulfites. These are additives in wine and some foods, such as processed potatoes and dried fruits. Shellfish packed in ice that has sulfites can pick up the sulfites from the ice.
• Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen
• Beta blocker medicines. These are prescribed for heart disease, high blood pressure, and migraine headaches.
Your Asthma Trigger Diary
Use the "Print on Demand" for a printer friendly version.
When to Seek Medical Care
Reasons to Call Doctor
Call your doctor when you feel the first change in your asthma status. Deal with a problem early to help prevent a severe problem.
• You have asthma and have a cold or a fever.
• You cough up mucus that is bloody-colored, green, or yellow.
• An asthma attack does not respond to your medication.
• Medication is not helping like it used to.
• Your peak expiratory flow (PEF) numbers are in the yellow zone.
• You have a harder time breathing or you are short of breath more often than before.
• You breathe faster than usual.
• Your asthma attacks are coming more often or are getting worse.
• You use your rescue medication more than 2 times a week.
Reasons to Get Medical Care Fast
• Your peak expiratory flow (PEF) numbers are in the red zone.
• You have a fever with heavy breathing.
• You have extreme shortness of breath. It may feel as if you can’t breathe at all. Or, you can’t say 4 or 5 words because you are so short of breath. Call 911!
• You cough so much that you can’t take a breath. Call 911!
• Your lips or fingernails are bluish in color. Call 911!
Focus on breathing slow and easy until you get medical care. Sit upright. Try to remain as calm and relaxed as you can.
Peak Flow Meters
These devices measure peak expiratory flow (PEF). PEF is the amount of air blown out after taking a deep breath. Your PEF readings can tell you and your health care provider:
• About asthma triggers
• If an asthma attack is starting. PEF is decreased with an asthma attack.
• If your medicine plan is working
• When to add or stop medicine
• How severe your asthma is
Use your peak flow meter, as directed by your doctor or health care provider.
Find Your Personal Best Peak Flow Number
Your personal best peak flow number is the highest peak flow number you can get over a 2-week period when your asthma is under good control. Good control is when you feel good and do not have any asthma symptoms.
Take peak flow readings:
• Twice a day for 2 weeks – when you wake up and about 10 to 12 hours later
• Before and after taking an inhaled beta2-agonist (if you take this medicine)
• As advised by your doctor or health care provider
The Peak Flow Zone System
Once you know your personal best peak flow number, your health care provider will give you the numbers that tell you what to do. The peak flow numbers are put into zones that are set up like a traffic light.
Green Zone (80 to 100 percent of your personal best number). This signals all clear. No asthma symptoms are present, and you may take your medicines as usual.
Yellow Zone (50 to 80 percent of your personal best number). This signals caution. You may need to take more of your asthma medicine(s) to treat your asthma. Or, your overall asthma may not be under control, and the doctor may need to change your asthma action plan.
Red Zone (below 50 percent of your personal best number). This signals a medical alert. You must take an inhaled beta2-agonist right away and call your doctor without delay if your peak flow number does not return to the Yellow or Green Zone and stay in that zone.
Treatment
The goals of treatment are to:
A. Prevent asthma attacks and control or treat asthma symptoms as they occur
B. Allow normal daily activities, including exercise
C. Promote restful sleep, free from waking up with asthma symptoms
D. Do A, B, and C with few or no side effects from asthma medications
E. Have no need for emergency medical care or to be hospitalized due to asthma
Treatment for asthma varies on how severe it is and how well it is controlled. Since a person’s asthma can change over time and the response to medications may be age-related, asthma treatment guidelines are given for three different age groups:
• 0-4 years
• 5-11 years
• 12 years and older
A good way to help you manage your asthma is to follow a written action management plan that you develop with your doctor or health care provider. Your plan should include:
• What to do daily to avoid and deal with your asthma triggers and what to do when you have an asthma attack
• Names and doses of medicines to take daily and when you have specific symptoms
• Reasons to contact your doctor or to get medical care fast
• Your plan should be tailored for your needs.
Keep a journal of your asthma symptoms. Include:
• When you had symptoms and what may have caused them. What you did to treat the symptoms. List the medicines you took, how you took them, and how much you took.
• Your peak flow meter readings. Record these before and after treatment steps.
• Results of the treatment steps you took
Self-Care
• Know your warning signs and peak flow zones so you can begin treatment early. Monitor your peak expiratory flow rates. (See “Peak Flow Meters”.)
• Keep your asthma rescue medicine handy.
• Get a yearly flu vaccine, as advised.
During an asthma attack:
• Sit up. Don’t lie down.
• RELAX. Keep calm. Focus on breathing slow and easy. Remove yourself from any stressors.
• Take the right amount of medicine, as prescribed in your asthma control plan. Call your doctor if you need to take more medicine than prescribed.
Avoid your asthma triggers
• Do not smoke. Do not allow smoking in your home, car, or around you. Avoid air pollution.
• Use bedding, flooring, paint, vaccum cleaners, toys, and other products that are “Certified Asthma & Allergy Friendly™.” (Search for items from www.asthmaandallergyfriendly.com.) It is especially helpful to use these products in your bedroom and/or:
– Sleep with no pillow or one your doctor suggests. Use a “dust-mite proof” cover to enclose your mattress and pillow (if you use one). Wash all bedding in hot water every week.
– Try not to keep stuffed animals in the bedroom. If you must, have only one that can be washed. Wash it in hot water once a week.
– Use curtains and rugs that can be washed often. Avoid carpeting, bed ruffles, and throw pillows.
– Get someone else to vacuum and dust once or twice a week. Use a vacuum with a HEPA filter or double-thickness bags. If you dust or vaccum, wear a dust mask.
– Reduce clutter in your bedroom. Store items in plastic containers with lids.
– It is best not to keep a TV, DVD-player, etc. in your bedroom. These, too, can collect dust.
• Put an air filter on your furnace or use a portable air purifier, such as one with a HEPA filter.
• Stay out of the cold weather as much as you can.
• Change and/or wash furnace and air conditioner filters on a regular basis. Keep indoor humidity below 60 percent.
• When you are outside in cold weather, wear a scarf around your mouth and nose to warm the air as you breathe in.
• Stop exercising if you start to wheeze.
• If you are sensitive to sulfites, don’t take foods or medicines that have them. Sulfites are in wine, some processed potatoes and dried fruits. Shellfish packed in ice that has sulfites can pick up the sulfites from the ice.
• Drink plenty of liquids (2-3 quarts a day) to keep secretions loose.
• Don’t take over-the-counter medications unless cleared first with your doctor or health care provider.
– Antihistamines dry nasal secretions and can cause airways to plug up by making secretions thicker. Antihistamines are also found in some cold remedies, so check labels.
– Some ulcer drugs increase the effects of some bronchodilators.
– Aspirin can trigger an attack in 3-5 percent of persons with asthma who have nasal polyps. Acetaminophen doesn’t have this effect.
Medications
Some medications are to be taken with an asthma attack. Other kinds are taken daily (or as prescribed) to help prevent asthma attacks.
Long-Term Control Medicines
These are taken daily (or as prescribed) to help prevent asthma attacks. Examples are:
• Corticosteroids. These help with the swelling in the airways that cause asthma symptoms. They can prevent, reduce, and/or reverse the swelling.
– Inhaled corticosteroids (ICSs). These are the most effective long-term medicines that control asthma. These are not the same as anabolic steroids that athletes may abuse.
– Oral corticosteroids. An example is prednisone. These are usually given for a short time, when a person’s asthma is not being controlled. Long-term use of these may be prescribed for persons with severe asthma that persists.
• Cromolyn sodium and nedocromil. These help prevent swelling in the airways when exposed to asthma triggers. They treat mild asthma that persists.
• LABAs (long acting beta2-agonists). These are bronchodilators. They relax the muscles of the airways. They are usually taken with ICSs to help control moderate and severe asthma and to help prevent symptoms during the night.
• Leukotriene modifiers. These prevent swelling in the airways and decrease mucus in the lungs. They treat mild asthma that persists or are combined with ICSs to treat moderate or severe asthma.
• Theophyllines. These are mild to moderate bronchodilators that may have mild anti-inflammatory effects.
• Medicines that modify the body’s immune response.
Quick-Relief Medicines
These are used to treat symptoms of an asthma attack. They help stop asthma symptoms before they get worse. They may be prescribed for use at other times, too, such as before exercising. Examples are:
• SABAs (short-acting beta-agonists). These are bronchodilators. They work quickly to relax the muscles of the airways and open up the air passages in the lungs and are the treatment of choice to relieve acute symptoms. They are usually taken in an inhaled form.
• Anticholinergics. These help prevent airway muscles from tightening and help keep mucus from forming. These are usually taken in an inhaled form.
With proper treatment and monitoring of symptoms, asthma can be controlled. People with asthma can live active and healthy lives.
This website is not meant to substitute for expert medical advice or treatment. Follow your doctor’s or health care provider’s advice if it differs from what is given in this guide.
The American Institute for Preventive Medicine (AIPM) is not responsible for the availability or content of external sites, nor does AIPM endorse them. Also, it is the responsibility of the user to examine the copyright and licensing restrictions of external pages and to secure all necessary permission.
The content on this website is proprietary. You may not modify, copy, reproduce, republish, upload, post, transmit, or distribute, in any manner, the material on the website without the written permission of AIPM.
2021 © American Institute for Preventive Medicine - All Rights Reserved. Disclaimer | www.HealthyLife.com