-
Women’s Health Issues





Breast Lumps, Cancer & Self-Exam
Feeling a lump in a breast can be scary. For a lot of women, the first thought is cancer. The good news is that 80 to 90% of breast lumps are not cancer.
Signs & Symptoms
-
•Solid tumors.
-
-Lipomas. These are fatty tumors that can grow very large. They are usually benign.
-
-Fibroadenomas. These lumps are round, solid, and movable. They are usually benign.
-
-Cancerous lumps. Often, these are firm to hard masses that do not move when felt. They are often an irregular shape.
-
•Cysts. These are fluid filled sacs. They are painful and feel lumpy or tender. Cysts can occur near the surface of the skin of the breast. They can also be deep within the breast. This second type may need to be tested with a biopsy to make sure the cyst is benign. Cysts can be very small and diffuse as in fibrocystic breast disease.
-
•Nipple-duct tumors. These occur within the part of the nipple that milk flows through. They cause a discharge from the nipple. These tumors should be removed by surgery. In rare cases, a bloody discharge from the nipple could be a sign of cancer.
Breast cancer often occurs without signs and symptoms. Early screening can help detect it.
Causes
Breast lumps are often caused by:
-
•Fluid filled sacs (cysts).
-
•Fibroadenomas.
-
•Fibrocystic changes.
Breast cancer results from malignant tumors that invade and destroy normal tissue. When these tumors break away and spread to other parts of the body, it is called metastasis. Breast cancer can spread to the lymph nodes, lungs, liver, bone, and brain.
Treatment
Benign breast lumps may go away if you breast-feed for many months or take a low-dose birth control pill. Prescribed medicines can get rid of severe breast lumps. These have side effects, though.
For Breast Cancer
-
•Surgery.
-
•Chemotherapy.
-
•Radiation therapy.
-
•Brachytherapy. This is the use of radioactive “seeds.” They are put into the breast at the site where the tumor was removed.
-
•Hormonal therapy.
-
•Stem cell or bone marrow transplant.
-
•Clinical trials.
Risk Factors
-
•Being a woman is the main risk factor. Yearly, about 180,000 women find out they have breast cancer. About 40,000 women die from it. {Note: Men can get breast cancer. Yearly, about 450 men in the U.S. die from breast cancer. Men should look for and report a breast lump or other change to their doctors.}
-
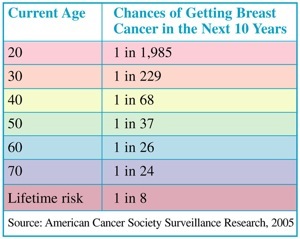
•Increase in age. The National Cancer Institute (NCI) has given these figures for women’s chances of getting breast cancer.










Self-Care / Prevention
For Cystic Breasts
-
•Do a breast self-exam monthly or as advised by your doctor.
-
•Get to and stay at a healthy body weight.
-
•Follow a low saturated fat diet. Eat soy foods.
-
•Limit or have no caffeine.
-
•Limit salt and sodium. This helps to prevent fluid buildup in the breasts.
-
•Don’t smoke. Don’t use nicotine gum or patches.
-
•Take an over-the-counter pain reliever. Take vitamin E, as advised by your doctor.
-
•Wear a bra that provides good support. You may want to wear it while you sleep, too.
Regular exercise promotes blood flow to the breasts.
For Breast Pain and/or Swelling (without Lesions or Redness)
-
•For pain due to trauma or surgery: Apply cold packs for the first 48 hours. Do this for 10 to 15 minutes at a time. Do it every 2 to 4 hours. After 48 hours, apply heat. Use a hot water bottle, warm shower, etc. Do this 10 to 15 minutes at a time. Do it 4 times a day.
-
•For pain not due to trauma or injury: Apply warm heat. Use a heating pad set on low or a hot water bottle. Do this for 30 minutes. Then apply an ice pack for 10 minutes. Repeat as often as needed.
-
•Take vitamins, as advised by your doctor.
-
•Take an over-the-counter medicine for pain and/or swelling. Take it as directed.
To Reduce the Risk for Breast Cancer
-
•If you are at a high risk for breast cancer, ask your doctor if you should take prescribed medicine, such as raloxifene.
-
•Eat a variety of fruits and vegetables and whole-grain breads and cereals.
-
•Get to and stay at a healthy body weight.
-
•Get 30 or more minutes of moderate activity most days of the week. Daily is better.
-
•Avoid X-rays that aren’t needed. Wear a lead apron when you get dental and other X-rays not of the chest.
-
•Limit alcohol intake to 1 drink per day, if any.
-
•Breast-feed your babies.
-
•To help detect breast cancer, do breast self-exams and have mammograms and professional breast exams, as advised by your doctor.
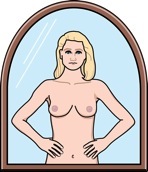
Breast Self-Exam (BSE)
Ask your doctor if and how often you should do a breast self-exam (BSE). Do a BSE at the same time each month to learn what is normal for you. The best time to do a BSE is within 3 days after your menstrual period stops. If you have gone through menopause, do a BSE the same day of each month.
Some lumpiness or thickening of the breasts is normal. Your “job” isn’t just to find lumps. It is to notice if there are any changes. If you have questions, ask your doctor. Don’t self-diagnose. If you find a change in a breast, a clear or bloody nipple discharge, or a lump, DON’T PANIC! Call your doctor or health care provider. Most lumps are not cancer.
Do a BSE in 3 Steps
-
1.In Front of a Mirror: Hold your arms at your sides. Look for changes in the shape of your breasts; dimpled, puckered, or scaly skin; or nipple changes or discharge. Raise your arms over your head. Look for the same things.
-
2.In the Shower: Lather your breasts with soap. Raise one arm. Move the pads of your 3 middle fingers, held flat, along the collarbone, over the entire breast (the tissue around the nipple, too) and your underarm area. Use your right fingers for your left breast and your left fingers for your right breast. Check for changes, lumps, knots, etc.
-
3.Lying Down: Place a pillow under your right shoulder. Put your right hand behind your head. Move the pads of your left hand’s 3 middle fingers, held flat, along the collarbone and over the entire right breast and underarm area. Massage the colored tissue around the nipple. Squeeze the nipple gently. Check for a clear or bloody discharge. Repeat all of these steps for the left breast.


Do you see or feel any lumps, dimpling, thickening, or puckering in a breast? Or, do you notice any changes in the size, shape, or contour of the breast?
With a family history of breast cancer, (especially in a mother or sister), are you concerned about breast cancer even if you don’t notice any problems?
Has a doctor diagnosed one or more lumps in your breasts as benign? If so, do you notice any new lumps? Have any lumps changed in size?
Do your nipples become drawn into the chest, invert totally, change shape, or become crusty from a discharge? Or, is there any nonmilky discharge when you squeeze the nipple of either breast?
Do you have any of these problems?
-
•Redness, swelling, and warmth in a breast.
-
•The skin on a breast appears pink, reddish purple, or bruised.
-
•Pain or constant tenderness in a breast.
-
•Cancer in one breast in the past. This increases the risk of cancer in the other breast or in another part of the same breast.
-
•Never giving birth or having a first full term pregnancy after age 30.
-
•Menstruation started before age 12. Menopause occurred after age 55.
-
•Family history of breast cancer for a woman whose mother, sister, or daughter has had it.
-
•Changes in BRCA1, BRCA2, and other cancer genes.
-
•One or more breast biopsies were done, especially if they showed certain changes in breast tissue.
-
•Long-term use of combined hormone therapy (estrogen and progesterone) after menopause.
-
•Eastern and Central European Jewish ancestry.
-
•Physical inactivity.
-
•Being overweight, especially after menopause.
-
•Race. Caucasian women have a greater risk than Asian, African American, Hispanic, and Native American women.
-
•Use of alcohol. The more consumed, the higher the risk.
Ask your doctor about your risk for breast cancer. You can also call 800.4.CANCER (422.6237) or access www.cancer.gov/bcrisktool for the Breast Cancer Risk Assessment Tool.
Treatment
For Breast Lumps
-
•Mammogram. This X-ray of the breasts can detect breast problems before they can be felt.
-
•Ultrasound. This tells whether the lump is fluid-filled (usually harmless) or solid.
-
•Needle aspiration. With this, a needle is put into the lump to remove fluid or cells.
-
•Biopsy. There are many types. A sample of breast tissue is taken and examined.
-
•Ductal lavage. Fluid is sent through a catheter to the milk ducts. Cells inside the milk ducts are collected and checked for the risk of breast cancer.
Questions to Ask



For more information, contact:
Cancer Information Service | 800.4.CANCER (422.6237) | www.cancer.gov




Copyright © 2009, American Institute for Preventive Medicine. All rights reserved.